 By Jill S. Bates, PharmD, MS, BCOP, FASHP, National PHASER pharmacy program manager, the Department of Veterans Affairs
By Jill S. Bates, PharmD, MS, BCOP, FASHP, National PHASER pharmacy program manager, the Department of Veterans Affairs
December 4, 2020
Precise, personalized and scalable: PGx as an essential tool in the CMM process
Let’s begin with our conclusion: To maximize medication optimization, we need to integrate pharmacogenomics into the process of comprehensive medication management (CMM).
Pharmacogenomics—PGx, for short—is the study of how a person’s genetic profile determines their body’s responses to specific medications. PGx testing allows for precisely fitted and delivered medical care based on the unique characteristics of an individual patient’s genetic profile, plus their lifestyle and environment. It is a tool to support CMM.
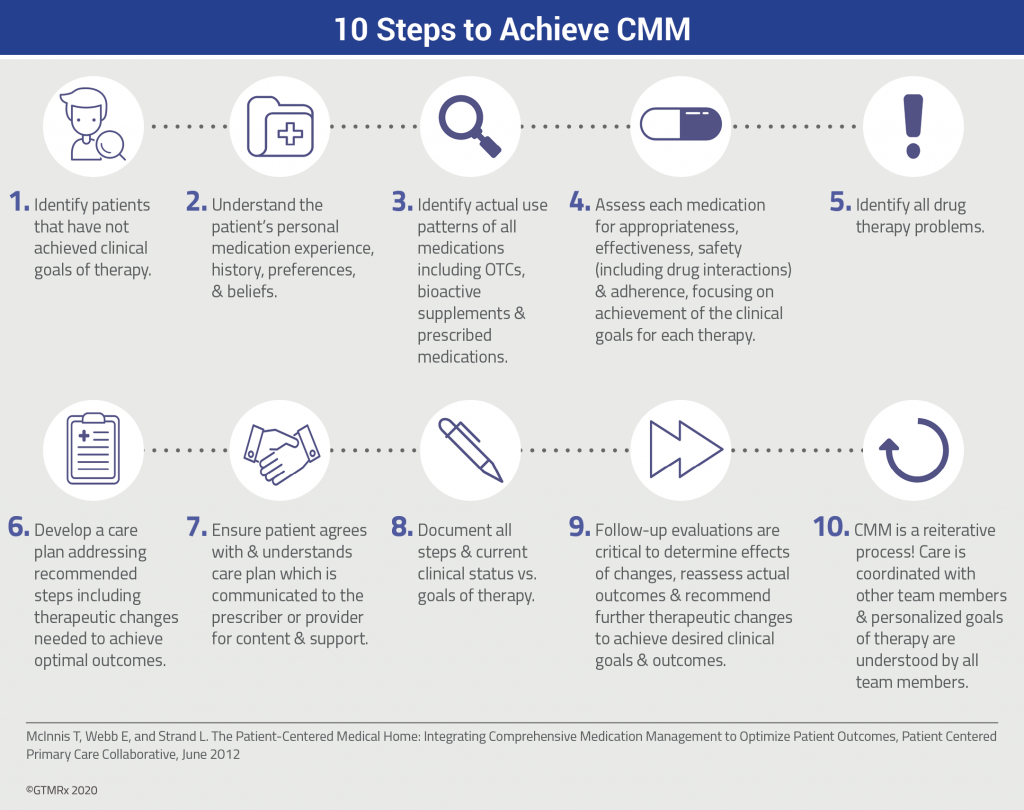
CMM is a care process. This patient-centered approach to optimizing medication use and improving patient health outcomes is delivered, at the point of care, by an interprofessional care team in collaboration with the patient.1
PGx meets CMM
PGx is a companion and complementary diagnostic tool that, when combined with the delivery of CMM services, helps address the problems of non-optimized medication use—especially adverse drug reactions and lack of efficacy.
It gives providers insight into how an individual patient’s genes may affect their response to certain medications. This allows providers to target correct therapies and mitigate harmful effects. By doing so, they can reduce total health care costs and optimize patient health.
The need for such a tool becomes clear when we recognize that roughly 90% of the population has at least one genetic variant that may affect the way they respond to medications, increasing the likelihood of side effects and/or treatment failure.2, 3
PGx as part of the CMM process provides a path to precise, personalized and optimized medication use.
Better together
We all recognize that pharmacogenomics itself is a valuable tool that can help us apply medication safety concepts and medication optimization strategies more precisely.
Now, think about what happens when you place that powerful tool in the context of CMM: You can gain so much more value regarding patient outcomes. Pharmacogenomics, paired with CMM, is extremely valuable—more so than either one deployed separately.
Not only are we looking at whether medications are safe and effective based on the literature and clinical guidelines, but we are also taking it down to the individual patient’s genetics to be able to find the optimal treatment. And we can do this at scale.
Barriers and gaps
Of course, as we’ve gathered the evidence, we’ve identified challenges. Specifically, we’ve found gaps in resources and accessibility.
We recognize the need for appropriate funding includes the monetary resources required to set up infrastructure to support pharmacogenomics in a CMM environment. But that’s just the most obvious. We also need human resources. Right now, physicians, pharmacists and other providers have varying levels of expertise when it comes to pharmacogenomics..
Lack of accessibility to pharmacogenomics represents the other yawning gap. It prevents us from obtaining the type of information we need to demonstrate clinical utility. Patients lack access to pharmacogenomics for two primary reasons. Often, they simply lack access to PGx testing itself. The other, as mentioned, is that their clinicians lack the expertise or knowledge to recommend it. Patients cannot obtain PGx testing if their providers don’t understand it..
Slowly, we are closing these gaps.
Precise and personal
PGx used in the context of CMM moves us to care that is precise and personalized. PGx testing makes treatment more precise. Using PGx as a tool within the CMM process makes care personalized. Integrating the two ensures we get medications right at scale, leading to better health and lower costs across populations..

The GTMRx’s Precision Medicine Enablement via Advanced Diagnostics Workgroup and Pharmacogenomics Payment and Policy Taskforce recently completed an evidence document that articulates the value of pharmacogenomics in the context of comprehensive medication management. In this blog post, Jill S. Bates, PharmD, MS, BCOP, FASHP. National PHASER pharmacy program manager for the Department of Veterans Affairs, offers insights into what the task force learned.
References:
[1] McClurg, M., Sorensen, T., Carroll, J. The Patient Care Process for Delivering Comprehensive Medication Management (CMM): Optimizing Medication Use in Patient-Centered, Team-Based Care Settings. CMM in Primary Care Research Team. July 2018.
[2] Ji, Yuan, et al. “Preemptive pharmacogenomic testing for precision medicine: a comprehensive analysis of five actionable pharmacogenomic genes using next-generation DNA sequencing and a customized CYP2D6 genotyping cascade.” The Journal of Molecular Diagnostics. 2016;18(3):438-445
[3] Van Driest, Sara L., et al. Clinically actionable genotypes among 10,000 patients with preemptive pharmacogenomic testing. Clinical Pharmacology & Therapeutics. 2014; 95(4):423-431.

